RETINA SPECIALIST IN THANE
Retina Specialist In Thane, The retina is a thin layer of tissue that lines the back of the eye on the inside. It is located near the optic nerve. The purpose of the retina is to receive light that the lens has focused, convert the light into neural signals, and send these signals on to the brain for visual recognition.
The retina processes light through a layer of photoreceptor cells. These are essentially light-sensitive cells, responsible for detecting qualities such as color and light-intensity. The retina processes the information gathered by the photoreceptor cells and sends this information to the brain via the optic nerve. Basically, the retina processes a picture from the focused light, and the brain is left to decide what the picture is.
Due to the retina’s vital role in vision, damage to it can cause permanent blindness. Conditions such as retinal detachment, where the retina is abnormally detached from its usual position, can prevent the retina from receiving or processing light. This prevents the brain from receiving this information, thus leading to blindness.
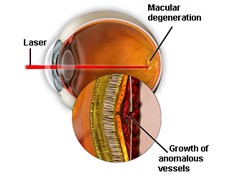
AGE RELATED MACULAR DEGENERATION
The disease affects the part of the retina called the macula, which is responsible for central vision. Vision loss from AMD typically occurs gradually and can affect both eyes at different rates. Even though macular degeneration can cause visual impairment, the disease usually does not cause peripheral (side) vision loss or lead to total blindness.
Types : The two common types of macular degeneration are “dry” and “wet.”
“Dry form” : The most common form of macular degeneration is caused by aging and thinning of the tissues of the macula. It develops slowly and usually causes mild vision loss. As this form of the disease develops, people often notice a dimming of vision while reading.


“Wet form” : Rare, and more severe. The wet form of the disease causes new blood vessels to grow beneath the retina, which leak fluid and blood, often creating a large blind spot in the center of the visual field. May progress rapidly causing significant central vision loss.
The causes of macular degeneration are not completely understood. Some scientists believe heredity may play a part, as well as UV light exposure, nutrition, and cigarette smoking. Studies are ongoing.
SYMPTOMS
- A dark area or a “white-out” appears in the center of vision.
- Blurred or fuzzy vision.
- Color perception fades or changes.
- Straight lines, such as sentences on a page or telephone poles, appear wavy or distorted.
TREATMENT
“Dry form” – There is no proven effective treatment for dry macular degneraation. Low vision rehabilitation can help those with significant vision loss to maintain excellent quality of life. High dose antioxidant vitamin therapy may help prevent some patients with dry macular degeneration from developing the wet form of the disease. “Wet form” – a variety of therapies are available for we macular degeneration; including intravitreal injection, photodynamic therapy, and rarely laser photocoagulation.
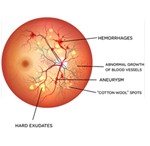
DIABETIC RETINOPATHY
The cells in persons with diabetes mellitus have difficulty using and storing sugar properly. When blood sugar gets too high, it can damage the blood vessels in the eyes. This damage may lead to diabetic retinopathy.
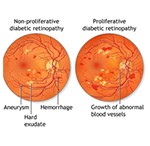
The two types of diabetic retinopathy are Proliferative diabetic retinopathy and Non Proliferative diabetic retinopathy.
PROLIFERATIVE DIABETIC RETINOPATHY
New, fragile blood vessels grow on the surface of the retina. These new blood vessels are called neovascularization, and can lead to serious vision problems, because the new vessels can break and bleed into the vitreous. When the vitreous becomes clouded with blood, light is prevented from passing through the eye to the retina.
Types : The two common types of macular degeneration are “dry” and “wet.”
This can blur or distort vision and frequently causes sudden and severe loss of vision. The new blood vessels can also cause scar tissue to develop, which can pull the retina away from the back of the eye. This is known as retinal detachment, and can lead to blindness if untreated. In addition, abnormal blood vessels can grow on the iris (the colored part in the front of the eye), which can lead to severe glaucoma.
Background or nonproliferative diabetic retinopathy – blood vessels in the retina are damaged and can leak fluid or bleed. This causes the retina to swell and form deposits called exudates.
Many patients may not notice any change in their vision when they develop this early form of the disease, but it can lead to other more serious forms of retinopathy that severely affect vision. Fluid collecting in the macula is called macular edema and may cause difficulty with reading and other close work.
TREATMENT
Good control of diabetes with intensive management and control of blood sugar will delay, and possibly prevent, both the development and progression of diabetic retinopathy. Patients with diabetic retinopathy frequently need to have special photographs of the retina taken. This series of photos is called fluorescein angiography.
Laser photocoagulation is one of the most common treatments for diabetic retinopathy. Focal photocoagulation consists of laser directed at the retina to seal leaking blood vessels in patients with background diabetic retinopathy. Panretinal photocoagulation consists of laser spots scattered through the sides of the retina to reduce abnormal blood vessel growth (neovascularization) and help seal the retina to the back of the eye in patients with proliferative diabetic retinopathy. This can help prevent retinal detachment. There is little recuperation needed after laser surgery for diabetic retinopathy. Laser surgery may require more than one treatment to be effective.
Vitrectomy surgery is performed for patients with very advanced proliferative diabetic retinopathy or retinal detachment. In vitrectomy, the surgeon removes the blood-filled vitreous and replaces it with a clear solution. This allows light to pass through the clear fluid to the retina, where the images are conveyed to the brain.
Pharmacotherapy : Increasingly, a variety of medications are being used to treat the manifestations of background and proliferative diabetic retinopathy.
These involve intravitreal injections of small amounts of medication into the eye.
The type of retinopathy, as well as the patient’s general health and eye structure will determine the kind of treatment needed and the type of anesthesia utilized.
FLASHES & FLOATERS
Some people may occasionally see small specks or clouds moving in your field of vision. These are called floaters. Floaters are actually tiny clumps of gel or cells inside the vitreous, the clear jelly-like fluid that fills the inside of the eye. While these objects look like they are in front of the eye, they are actually floating inside. When people reach middle age, the vitreous gel may start to thicken or shrink, forming clumps or strands inside the eye. The vitreous gel pulls away from the back wall of the eye, causing a posterior vitreous detachment.
Posterior vitreous detachment is more common in people who :
• Are nearsighted
• Have undergone cataract operations
• Have had YAG laser surgery of the eye
• Have had inflammation inside the eye
When the vitreous shrinks, it tugs on the retina, creating a sensation of flashing lights. The flashes of light can appear off and on for several weeks or months. As we grow older, it is more common to experience flashes.
As the shrinking vitreous gel pulls away from the wall of the eye, it can cause a retinal tear in places where the vitreous gel sticks too tightly to the retina. This sometimes causes a small amount of bleeding in the eye that may appear as new floaters. A torn retina is always a serious problem, since it can lead to a retinal detachment.
MODES OF TREATMENT
INTRAVITREAL INJECTIONS : Intravitreal Injections are increasingly important for patients with retinal diseases. Many of these treatments are directed at inhibiting Vascular Endothelial Growth Factor (VEGF). Vascular Endothelial Growth Factor (VEGF) is a substance made by cells that stimulates the growth and leakage of abnormal new blood vessels. VEGF plays a large role in the development of wet age-related macular degeneration (AMD) and other retinal vascular diseases. Multiple new treatments for wet age related macular degeneration that block VEGF are now clinically available. These treatments are given as a series of injections into the eye (intravitreal injection). Intravitreal injections are performed in the office, using an anesthetic to minimize patient discomfort and antiseptic to minimize the risk of infection. Patients are able to continue with all normal activities after an injection. In many cases, repeated injections are necessary to achieve the desired effect.
MACUGEN : Was the first of these agents to become available, gaining FDA approval in December of 2004. Macugen binds and inactivates a VEGF subtype (VEGF-165) thought to be most important in disease progression.
AVASTIN : Is an anti-VEGF treatment that is FDA approved for intravenous use in metastatic colon cancer. Due to its similarity to other anti-VEGF agents used in macular degeneration and its widespread availability, Avastin has become commonly used by retina specialists in small doses as an intravitreal injection. Avastin is used in an off-label (non-FDA approved) fashion for treating wet age related macular degeneration, diabetic retinopathy, and retinal vein occlusions. Although mounting evidence has demonstrated the effectiveness and safety of Avastin, further trials are underway to investigate the use of Avastin inside the eye.
LUCENTIS : Is the newest and most effective anti-VEGF agent approved by the FDA for the treatment of wet age-related macular degeneration (AMD). In 2 clinical trials, a majority of patients receiving monthly injections of ranibizumab maintained their vision. Moreover, approximately one-third of ranibizumab patients had improvements in vision at 12 months. Lucentis is the first treatment for wet macular degeneration to show an average improvement in visual acuity after one year of treatment in clinical studies.
SURGICAL TREATMENT
Vitrectomy : A sophisticated microsurgical technique in which the vitreous gel is removed from inside the eye with a small, specialized cutting device, an operating microscope to look into the eye, and microsurgical instruments. The vitreous gel is then replaced with a clear saline fluid. Vitrectomy is performed for many conditions including retinal detachment, diabetic retinopathy, macular pucker or hole, hemorrhage or infection inside the eye, and ocular trauma. Vitrectomy is usually performed under local anesthesia.
Scleral Buckle : A special plastic material is placed around the outside to help close off (or “buckle”) retinal tears in patients with a retinal detachment. We also have specialized equipment that enables us to repair certain retinal detachments in the office without the need for hospitalization or scleral buckling.